
Last time on the blog, I talked about culture change. Culture change takes bold leadership—leaders who solve problems by putting quality first. Easy to say and not always easy to do.
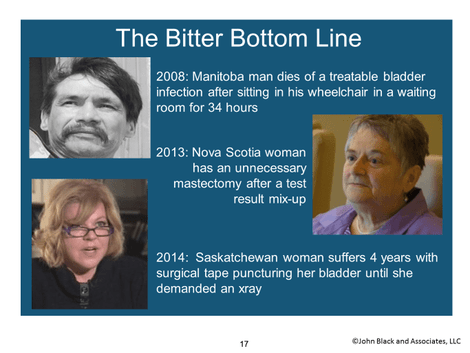
Sometimes those leaders are patients and patients’ family members. When patients are bold enough to speak out, hospital caregivers better listen. Why? Because including patient voices can prevent future tragedy. I like this definition for tragedy from Merriam-Webster: “a very bad event that causes great sadness and often results in someone’s death.”
Watch this video of a young mother's experience of tragedy:
Sometimes those leaders are patients and patients’ family members. When patients are bold enough to speak out, hospital caregivers better listen. Why? Because including patient voices can prevent future tragedy. I like this definition for tragedy from Merriam-Webster: “a very bad event that causes great sadness and often results in someone’s death.”
Watch this video of a young mother's experience of tragedy:
Here’s how this mother’s story ended: An air ambulance was finally arranged for the baby. The mother had been trying to get her baby help for more than a week. She was frantic – her new baby died seven minutes after the helicopter landed.
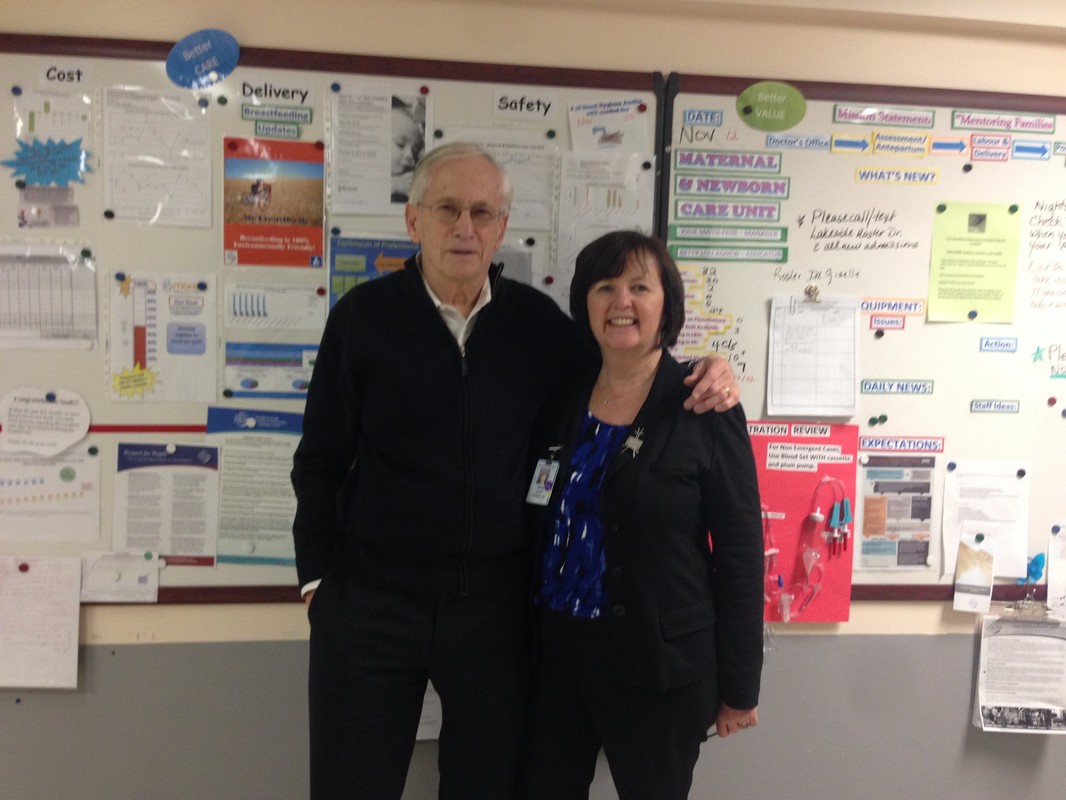
The reason this mother could be as positive as she seemed in the video was that time had passed. When I spoke with her she wanted to tell her story, she asked that she be videotaped. She’d been invited to participate in a Lean 3P Clinic design event JBA conducted in Saskatchewan. Even though her concerns were discounted in more than two dozen interactions with the healthcare system, she was enthusiastic about trying to make sure such tragedies don’t happen again. She showed tremendous courage, and decided to become part of the solution for others.
Don’t misunderstand me, I’m not calling out Saskatchewan, there are many wonderful positive stories in that great Province. What about Seattle you might ask? Here in Seattle we saw another tragic example of a patient’s voice being silenced. Talia Goldenberg went in for elective surgery to fuse her neck, due to a rare joint-tissue disorder. After the surgery, her father, an MD, could tell something was seriously wrong with his daughter’s airway. Nurses moved her to the ICU. But then, in a critical mistake, the surgeon who performed the surgery ignored the father’s pleas and removed Talia from the ICU. Later, Talia suffocated to death in front of her father. If the surgeon had listened to Talia’s father instead of his ego, Talia would have survived. Tragedy.
The reason this mother could be as positive as she seemed in the video was that time had passed. When I spoke with her she wanted to tell her story, she asked that she be videotaped. She’d been invited to participate in a Lean 3P Clinic design event JBA conducted in Saskatchewan. Even though her concerns were discounted in more than two dozen interactions with the healthcare system, she was enthusiastic about trying to make sure such tragedies don’t happen again. She showed tremendous courage, and decided to become part of the solution for others.
Don’t misunderstand me, I’m not calling out Saskatchewan, there are many wonderful positive stories in that great Province. What about Seattle you might ask? Here in Seattle we saw another tragic example of a patient’s voice being silenced. Talia Goldenberg went in for elective surgery to fuse her neck, due to a rare joint-tissue disorder. After the surgery, her father, an MD, could tell something was seriously wrong with his daughter’s airway. Nurses moved her to the ICU. But then, in a critical mistake, the surgeon who performed the surgery ignored the father’s pleas and removed Talia from the ICU. Later, Talia suffocated to death in front of her father. If the surgeon had listened to Talia’s father instead of his ego, Talia would have survived. Tragedy.
At JBA, we make patients part of the transformation process. Here’s Heather Thiessen’s experience collaborating with hospital staff:
“I was part of a design group for the adult ED. It was my second Lean event and so exciting. In my many years as a patient, I had never been asked what I think. But who better to help when making changes? We see waste and safety issues daily, but who do you tell? More often than not, our voices in the past would be hushed or we’d be told we don’t know what we are talking about.
Studies have shown that families are often the first to see when a patient is failing health-wise. When that’s not heard, that patient is in danger. My husband is a prime example. When I was hospitalized for my myasthenia, he could recognize when I was not doing well, especially when he had been away at work. He had that fresh perspective and knew if something was not right. He would ask the nurses, “What is wrong with Heather?” He knew right away if something was out of my normal. Often, if his observations were dismissed, I would have a trip to the ICU that evening.
This is why the patient and family voice is so critical. We were able to bring our perspective to the table, and what was so amazing in the ED design event is that everyone’s “professional hat” was not brought to the table. Instead it was, “How can we all come together to make sure we build a patient- and family-centered, safe hospital?” I am still part of the group that meets regularly on updates and decisions, with the patient and family voice first and center.
As a patient and family advisor I was so respected, and my thoughts and ideas were acted upon — and that was a distinct change from the past. Patients, for the first time in my 20 years of being a patient in the region, were seen as a valuable part of the team.”
Patient voices help hospital staff see problems before they become tragedies. Patient voices come up with solutions that hospital staff can’t.

 RSS Feed
RSS Feed